Abstract
Chronic lymphocytic leukemia (CLL) is characterized by a variety of genomic aberrations including the chromosomal abnormalities del11q, del13q and del17p, tri12, as well as the 2pgain. The 2pgain is frequent in symptomatic CLL (16%), and is associated with poor prognostic factors (del11q, unmutated IGHV) and drug resistance. At least two minimal regions of gain 2p15-16 and 2p24 have been identified. The aim of the present study is to describe the relationship between 2pgain and other key CLL chromosomal abnormalities and to investigate the evolution of the 2pgain under therapeutic pressure.
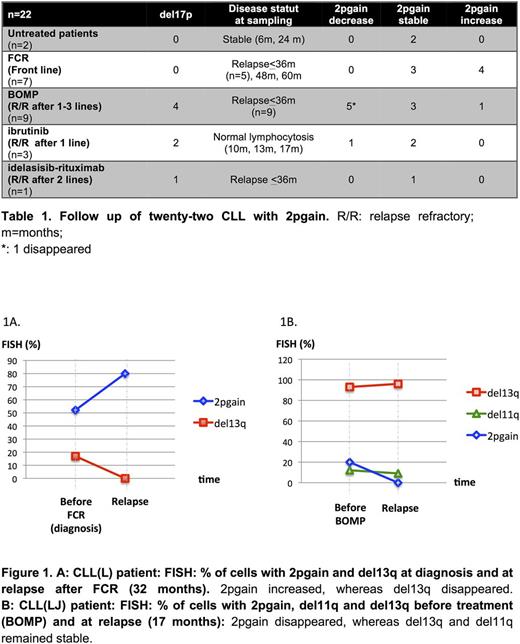
We have collected data for 64 CLL patients (pts) with 2pgain detected by karyotype (k) and/or extensive fluorescence in situ hybridization (FISH). In all pts K and extensive FISH have been performed, including the 4 classical CLL probes and probes encompassing MYCN (2p24), REL (2p16) XPO1 (2p15), and BIRC3 (11q22) genes. The IGHV status was also determined. Longitudinal cytogenetic analyses were available for 22/64 patients.
Eighty three percent (53/64) of patients with 2pgain were male, with a median age at diagnosis of 60 years (range: 42-80). Out of 52 successful K, 21 (40.4%) were complex (C) (≥3 abnormalities) (9/52, 17.3%) or high C (≥5 abnormalities) (12/52, 27.1%). The 2pgain was clearly identified in 13/52 (25%) K, and was due to a duplication in the short arm of chromosome 2 in 5 cases, while in the remaining cases it was fused to chromosomes 4, 8, 13, 20, 22 and most frequently to chromosome 18 (5/15, 38.4%). In the majority of cases 2pgain was accompanied by other aberrations, including 56.2% del13q, 45.3% del11q, 21.8% del17p and 1.5% tri12. The IGHV status was unmutated in 51/56 (91%) patients.
Regarding the 22 patients with longitudinal samples, the median number of samples was 3 (range 2-5), and the median follow up (FU) was 8.6 years (range 4-26). Among them, 20 patients required treatment, with a median time from diagnosis to treatment of 26.3 months (1-72). Seven patients died, with a median OS of 9.3 years (range 4-26). Investigating the 2pgain in more detail, we found that the three oncogenes XPO1, REL and MYCN were gained in the same proportion of cells in the large majority (68.2%) of cases. However, in 7/22 (31.8%) CLL, we observed a divergence in the gain of 2p15-16 (XPO1/REL) and 2p24 (MYCN) regions. In 6/7 cases, the 2p15-16 region was gained in more tumor cells than 2p24, including 3 CLL without any detectable gain of MYCN ; conversely in one patient, 2p24 was gained in a higher percentage of cells than 2p15-16. Regarding the 11q deletion, ATM and BIRC3 were both deleted in 10/12 (83%) cases. Only 2 cases had a deletion involving ATM only; no case of simple BIRC3 deletion was observed.
During the evolution, the 2 untreated patients had a stable % of 2pgain, with a FU of 6 and 24 months. A median of 3 lines of therapies was used in the 20 patients requiring treatment. Thus, in our study, we have compared cytogenetic data for each line before treatment and at relapse (Tab 1). Among the 20 patients: i. Seven were treated with fludarabine/cyclophosphamide/rituximab in front line. Time to relapse was within 3 years in 5 patients, and the 2pgain remained stable (3/7) or increased (4/7) (Fig 1A); ii. Nine pts were treated with bendamustine/ofatumumab/methylprednisolone (BOMP), after 1 to 3 lines of previous therapies; the 9 cases relapsed (including 1 death) within 3 years. At relapse, the 2pgain decreased (4/9) or disappeared (1/9) (Fig 1B), remained stable in 3 cases, and increased in one patient. Of note, 4/9 patients had a del17p, which remained stable or increased; and iii. Three patients were treated with ibrutinib: the 2pgain decreased in one patient after 11 months, and remained stable in two patients, despite a normal lymphocyte count at 13 and 17 months. Finally only one patient received R/idelalisib after 2 previous lines, and died at 25 months, with a stable 2pgain.
Conclusion: In the era of precision medicine, our results suggest that in addition of the other classical prognostic factors, 2pgain has to be specifically evaluated in CLL before deciding the treatment strategy. As 2pgain could be overlooked by conventional karyotype, we suggest searching systematically this abnormality by FISH with at least two sets of probes (XPO1/REL and MYCN). The majority of the drugs seem not to be effective on the elimination of the 2pgain clone, but the BOMP regimen could be an option. No data are available regarding BCL-2 inhibitors in this setting.
Leblond: SERVIER: Honoraria, Membership on an entity's Board of Directors or advisory committees; GILEAD: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; JANSSEN: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; BMS: Honoraria; ABBVIE: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; ROCHE: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; NOVARTIS: Honoraria, Membership on an entity's Board of Directors or advisory committees. Guieze: GILEAD: Other: Educational Presentation; ABBVIE: Other: Educational Presentation; JANSSEN: Other: Educational Presentation. Tournilhac: Abbvie: Honoraria, Other: Travel funding; GILEAD: Honoraria, Other: Travel Funding, Research Funding; ROCHE: Honoraria, Other: Travel funding, Research Funding; AMGEN: Other: Travel funding, Research Funding; Janssen: Honoraria, Other: travel funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal